Inflammations under control, but still abdominal pain
Many people with chronic inflammatory bowel diseases such as Crohn's disease or ulcerative colitis continue to experience persistent abdominal pain. They feel that they are not getting enough help for their pain, even when their inflammations are well managed. Because there is still little known about this form of chronic pain, gastroenterologist Dr. Zlatan Mujagic of the Maastricht University Medical Center+ will conduct research to better understand it. For this, he has received the prestigious Clinical Fellowship Research Grant from ZonMw.
About 90,000 Dutch people have Crohn's disease or ulcerative colitis, which are chronic inflammatory bowel diseases (IBD). Even if the inflammations in IBD are well treated, up to 40% of patients experience chronic abdominal pain. This pain is difficult to treat, but has a major impact on their quality of life.
Better insight
Little is still known about the mechanism behind chronic abdominal pain in IBD, Mujagic explains: "With this research, we want to get a better insight into it and determine which factors contribute to the persistence of the pain, while inflammations are under control. We think that factors such as diet, previous medication use, stress, and social factors play a role. If we gain more insight into these factors, we can take them into account in treatment."

Gastroenterologist Dr. Zlatan Mujagic
MyIBDcoach
Twenty Dutch hospitals are using myIBDcoach, which was developed and initiated together with the MUMC+. This is a digital method that helps patients monitor their own health status and learn to manage IBD. The method also offers better insight into the patient's health status for healthcare providers. About 7,000 patients use myIBDcoach and regularly answer questions about symptoms, medication, healthcare usage, and lifestyle. They will be asked to give permission to share this data from myIBDcoach for scientific research, allowing Mujagic to study the developments and mechanisms behind chronic abdominal pain.
Personalized approach
Based on the improved insight into pain, Mujagic hopes to make a personalized approach possible: "Because various factors play a role in chronic abdominal pain, we do not think that developing a single pain treatment will work. We hope to ultimately offer tailored solutions, such as a combination of medication and support from a dietician if diet plays a significant role, or social work if social factors are crucial."
Inflammatory Bowel Diseases (IBD)
IBD is the collective name for chronic bowel diseases, which includes Crohn's disease and ulcerative colitis. The Department of Gastroenterology and Hepatology at Maastricht UMC+ has a dedicated IBD team consisting of various healthcare professionals, including gastroenterologists, gastroenterology fellows, nurse practitioners, biological nurses, research nurses, surgeons with a focus on IBD, and researchers. The IBD team also collaborates with other disciplines such as dietetics, medical social work, clinical psychology, and psychiatry.
Holistische benadering
The Department of Gastroenterology of the MUMC+ places great emphasis on the human aspect of patient care. Mujagic explains, "Many patients experience a so-called patient-doctor gap: the doctor treats a condition, but the patient still goes home dissatisfied. That is why we choose a holistic approach at MUMC+." The department conducts research on IBD, IBS, and other related conditions with a focus on the patient's well-being as a whole.
Patient Thijs' story (31 years old)
When Thijs (not his real name) found out that gastroenterologist Zlatan Mujagic was going to investigate persistent pain in IBD patients, he wanted to share his story about IBD and pain.
"Although I have been diagnosed with Crohn's disease since the age of 21 and have become accustomed to having abdominal pain, it was not until I was 29 that my real struggle with IBD began. In 2020, I had to be admitted to the hospital due to a flare-up of my Crohn's disease. After a weekend of pain medication, I was subjected to tests and investigations familiar to every colitis or Crohn's patient. In the following week, I was given Prednisone and started to feel better. However, there was something else: I couldn't eat solid food without experiencing intense stomach pain and cramps. The doctors said that this would go away after a few weeks.
But it didn't. Months went by, and the pain remained the same, or even got worse when I tried to eat solid food prescribed by dieticians. In the first few weeks, I lost a lot of weight, and this trend continued. I was readmitted to the hospital, and the same tests were performed, but nothing was found. My Crohn's disease was under control. I was sent home with medication to help with stomach and abdominal cramps. The result was that my intestines started to work too slowly, and I had to take a lot of laxatives, which caused even more pain. Oxycodone was prescribed, a powerful painkiller, because they didn't know how to treat the pain. To be honest, this medication worked very well for the pain. It gave me a chance to take a break from the pain. However, it also stopped the movement of my intestines and stomach, and I had to have my stomach and intestines flushed twice a week. This went on for months while I was shuttled back and forth between different academic hospitals, always with the same question: how to deal with this pain? And always being told that my Crohn's disease was under control. I'm sure I'm not the only one in this situation, and people with IBD will recognize, and above all, feel, the image visualising the patient-doctor-gap.
After almost two years, I was referred to Maastricht UMC+. The first conversation with Dr. Mujagic was a relief right away. I felt that someone was really trying to understand me and not just looking at the state of my small and large intestine. Fortunately, his schedule allowed for a thorough discussion. At the end of the conversation, he explained to me that the current procedure for relieving pain in IBD with strong painkillers like Oxycodone is not uncommon, but that long-term use of these painkillers disrupts intestinal movements. Moreover, prolonged use of these painkillers only stimulates the brain to feel more pain. Mujagic gave me a clear picture of the coming months, gradually reducing and stopping these painkillers and starting medication to reduce the sensitivity of my intestines and promote movements. In addition, he made appointments with other specialists to take a holistic approach to my case. To my surprise, he walked into the waiting room of the other specialist and did a warm handover, so that everyone was on the same page. Now, eight months later, my diet consists of partially liquid and solid food. Moreover, having pain has become a rare occurrence instead of being constantly present. I wish this for everyone with IBD."
This article was previously published by Maastricht UMC+.

"Many patients experience a so-called patient-doctor gap: the doctor treats a condition, but the patient still goes home dissatisfied. That is why we choose a holistic approach at MUMC+."
- Gastroenterologist dr. Zlatan Mujagic
Also read
-
Drawing blood, inserting an IV, or looking into the ear; even seemingly simple medical procedures can cause anxiety, pain, and stress in children. According to pediatric intensivist Piet Leroy, comfort and trust are just as important as the medical treatment itself. Therefore, he is researching how...
-
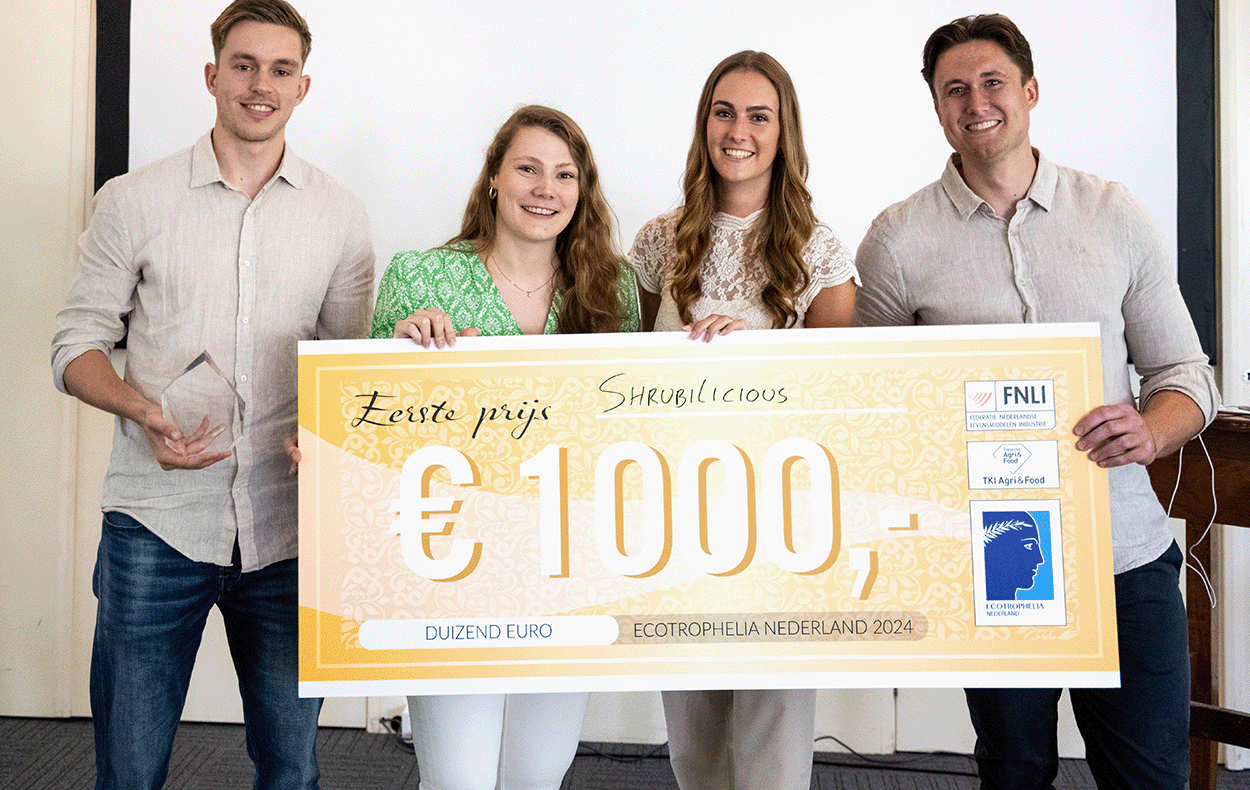
Maastricht University students have won the Dutch final of the student competition Ecotrophelia, a drinking vinegar based on apple cider vinegar, fruit and herbs.
-
In the upcoming months, we’ll share tips on Instagram for our students on how to live a healthier life. Not just a random collection, but tips based on actual research happening at our faculty. The brains behind this idea are Lieve Vonken and Gido Metz, PhD candidates at CAPHRI, the Care and Public...