How stemcells, a centrifuge and a 3D-printer prevent an amputation
As a scientist, it is your dream to develop or discover something within your domain of expertise that is of great significance. For Martijn van Griensven, professor of Regenerative Medicine at the Faculty of Health, Medicine and Life Sciences that dream came true. In the summer of 2020, a successful operation was performed using a method co-developed at Maastricht University. A method that could prevent the lower leg amputation in a patient and ensure that the patient can use his leg again after years of problems and pain due to a bone fracture. The operation was the result of a successful collaboration between Martijn van Griensven and trauma surgeon Martijn Poeze. The story of a breakthrough.
“When a person breaks a bone, the fracture can heal by itself. The body is able to close the gap itself. However, this only works successfully if the fracture is relatively small. In case of larger fractures, it is difficult for the bone cells to repair.
Lazy cells
Through research Martijn van Griensven knows that cells can be lazy. They can mend a small fracture but when it gets serious, cells don’t do much. The body will then try to send original cells from the bone marrow to the area of the fracture. These also contain stem cells, which are needed to create new bone. The stem cells are located far away from your bones in your leg. So they have to travel a long way in your body. This is a very difficult process. In the case of the patient who has now undergone surgery with the new method, the gap in his shinbone was 15 centimetres long. An immense job for bone cells and stem cells to complete. Van Griensven: “Compare this with the distance between Katwijk and England. You know that there is land at the other side of the water, but you don’t see it. This is also the case with such huge bone fractures: it seems an impossible task to bridge them. The question arises: is there anything that we can create outside the body – in the lab – that we can place in the hole that will allow the fracture to heal and the patient to put weight on the bone again?
Fundamental research
Van Griensven conducted research for many years. He studied how bone cells work, what bone cells look like, and what they are made of, as well as the question: why do large bone fractures not heal? Fundamental research is what we call it in science. “Bones are largely made of calcium. However, they are not solid: there are many small holes in it. In these small holes, the bone cells ‘live’ so to speak. Think of it as the cave dwellings you find in certain regions of Spain. Holes in the mountains where people have made houses. This is how you can see a bone with bone cells in our body.”
Transnational research
We wanted to develop exactly such a porous material out of calcium. This can be referred to as the second step in the scientific research process: translational research. In this phase, a researcher is searching for solutions to a problem, in this case in patients at the clinic. “We managed”, explains Van Griensven. “We made a biodegradable plastic skeleton with cavities and covered the whole thing with a layer of calcium, very similar to our bones. The biodegradable plastic skeleton is necessary, because the calcium would crumble and collapse too quickly. You also need a solid foundation for your house.”

Martijn van Griensven (46) is professor of Regenerative Medicine at the Faculty of Health, Medicine and Life Sciences of Maastricht University, and head of the department cBITE (Cell Biology-Inspired Tissue Engineering) at MERLN, Institute for Technology-Inspired Regenerative Medicine. He studied in Leiden and he lived and worked in Germany and Austria for 23 years. He has conducted research in the areas of traumatology and orthopaedics, including molecular and cell biology as well as regenerative medicine. In 2002, he became the youngest professor ever in Germany.
His heart belongs to traumatology. “That remains my subject. There is still so much to discover. I have a lot of knowledge of bone, cartilage and cruciate ligaments. At the university, we also work on tissue research in the eyes and pancreas of patients with diabetes. These subjects are new to me, but I love it. At Maastricht University, we share our knowledge and therefore we will ultimately create even more impact for patients in the clinic. With successful research, and the application of what we discover in medicine. That is the most beautiful thing there is.”
Clinical research

There was imitated bone material, there was knowledge about stem- and bone cells, and there was the patient with the large bone fracture. How to combine these aspects successfully? The last phase of scientific research began: clinical research. A centrifuge and a 3D-printer were key. “The question was: ‘can we extract the stem cells we need to make new bone from the bone marrow and then place them into the artificial bone we created.
We found the answer in a centrifuge. We had learned that if you spin the bone marrow in a centrifuge at a high speed, you could extract large amounts of stem cells. That is how the operation started. In the operating room, we collected bone marrow from the patient. We put the bone marrow in a centrifuge for thirty minutes. This allowed us to separate the stem cells.
We placed these stem cells in the reconstructed bone material. We had that piece of bone printed by a 3D-printer in Singapore. There, such a process can take place with a very clean printer, which of cause is crucial for such an operation like this. You want to keep the risk of infections as low as possible. We recreated the piece of the bone using a CT scan of the gap with the surrounding bone and the piece of bone in the patient’s other leg, that was still intact. It’s like building with Lego blocks, every edge, every piece has to fit.
Operation successful?
After the replicated piece of bone had been placed in the hole, and the stem cells were injected into the holes, the operation was completed. Then the waiting started. “What you hope for is that the cells feel well enough to start making new bone themselves. The replicated bone is degradable. Over the next two to three years, the cells have to start making new bone and the recreated piece of bone will disappear."
After six weeks, we could make the first X-ray, and with it came the redeeming image. Little dots were visible; the cells had started to create new bone. Recently, just 5 months after the operation, it was clear that about half had already become new bone. ‘Over the moon’, Van Griensven describes his feeling on seeing the first images. “We built a kind of walkway to England, which allowed the cells to crossover. It is unbelievable that we have succeeded in this, and that we were able to give a person his life back as it used to be before his accident. We have made a bridge between fundamental research and the patient in the clinic. “This is the purpose of our work.”
Second patient
Collaboration between the university and the clinic continues: after this successful operation in the Netherlands, this method will be applied to a second patient in 2021. Van Griensven also attends weekly meetings of the surgical team in the clinic. This way, research and clinic know how to find each other, can anticipate problems and find solutions.
New research objective
And Martijn van Griensven? The researcher in him has a new goal: to come up with a solution for better healing of torn-off tendons and (cruciate) ligaments. “Because a ligament or tendon is elastic and the bone to which it is attached is hard, it turns out to be very difficult to reattach the two properly and permanently after a problem. Where two components meet, it is delicate. We are currently researching how we can properly reattach soft tendons or ligaments to the hard bone. That way, we can help many relatively young people who experience this. I hope to realize another successful operation before my retirement. We shall see. As it stands, I will be working on this for the next fifteen years.
text: Antoinette van der Vorst
Also read
-
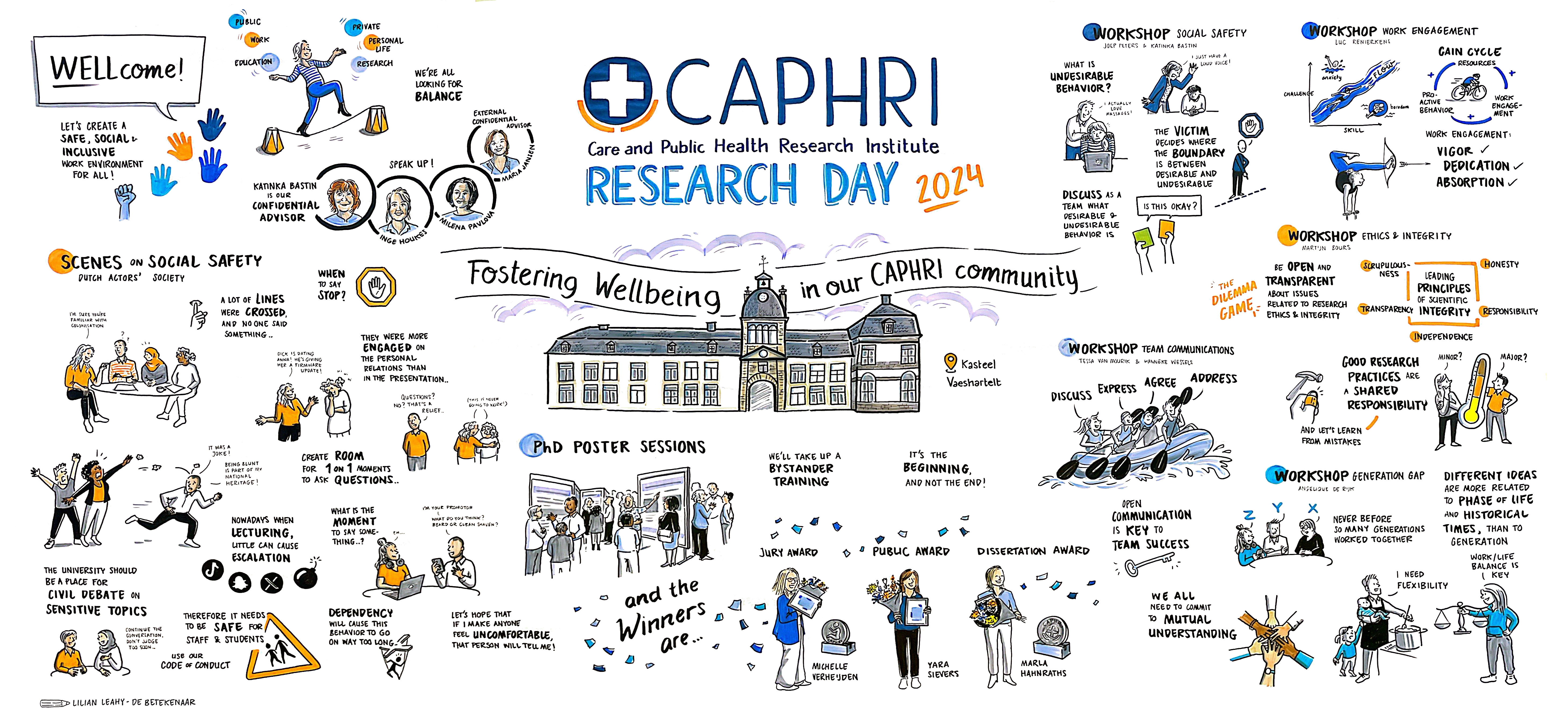
We are happy to have welcomed you on June 19th during our annual CAPHRI Research Day 2024 with the theme “Fostering Wellbeing in our CAPHRI Community”. We look back at yet another successful edition, where we got the chance to meet, interact, discuss, reflect and learn. Thank you for your presence...
-
As of February 1st, 2024, emeritus professor Maria Jansen has been appointed as an independent external confidant for PhD candidates at FHML/Maastricht UMC+.
-
Jos Schols has been honored with the prestigious GRZ Award 2024 for his contributions to short-term care, particularly in geriatric rehabilitation.