Real world data to prevent flares and improve health of patients with IBD
Division 2: Liver and Digestive Health
Department of Gastroenterology - Hepatology, MUMC+
Background
More than half of the people in Western countries have at least one chronic disease. The cause of chronic conditions is in most cases complex and multifactorial. Environmental factors, lifestyle (e.g. nutrition, exercise) and psychosocial factors (e.g. social support, adherence) have a major influence on both the clinical course of the disease and the subjective health of patients, measured with patient reported outcome measures (PROMs).
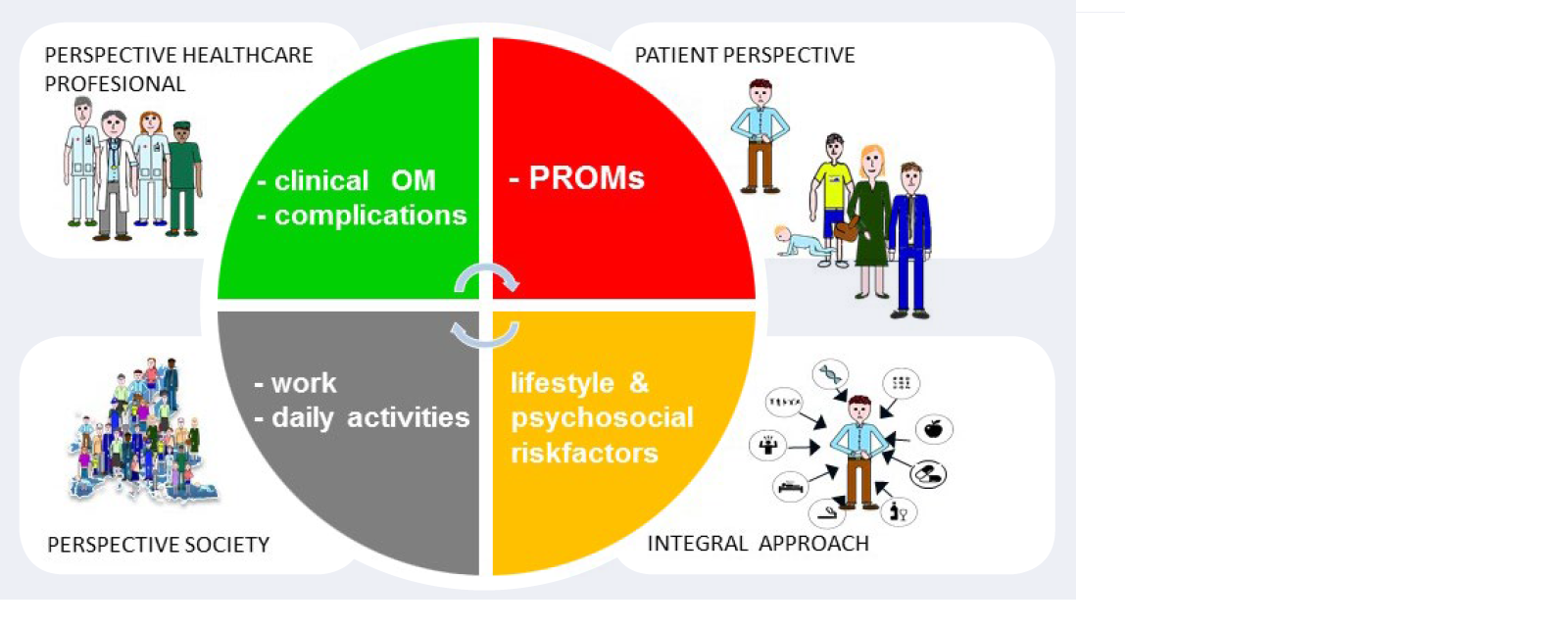
Quality of care is the degree to which the care provided succeeds in improving health. The best possible care provides optimal outcomes for all parties in the health care system; the patient, healthcare professional, regional care network and the society, with the available resources. Therefore, registering and reporting of all outcomes is necessary to measure quality of care and evaluate the effect of interventions (Figure 1). Digitisation in healthcare, in particular the introduction of electronic patient files and Telemedicine enables registration of all these outcomes within the primary care process.
The inflammatory bowel diseases (IBD), Crohn’s disease and ulcerative colitis, are chronic conditions characterized by recurrent inflammation of the intestinal mucosa. There are more than 90,000 people with IBD in the Netherlands and the incidence is rising [1]. Like other chronic diseases, IBD has a complex aetiology and a heterogeneous clinical presentation and disease course. There is no curative treatment, no available drug is effective for all patients, and most drugs can cause serious side effects. State-of-the-art clinical stratification does not sufficiently predict the response to drugs and there are no reliable molecular markers. With traditional disease, management based on the treatment of symptoms and a ‘step-up trial and error’ drug introduction structural bowel damage caused by insufficient control of chronic inflammation is still common and negatively impacts the quality of life [2]. To improve the long-term course, new drugs were developed and new treatment goals and strategies were introduced. It is however unknown how quality of life, disability and quality of care have evolved in parallel with these innovations over the past ten years or if the interventions are cost-effective.
As with other chronic conditions, there frequently is a perception gap between doctors and patients; people with IBD often have disabling complaints, while the doctor believe, the disease is in remission. It is therefore important in addition to monitoring the clinical outcomes; mucosal inflammation and complications to measure the subjective burden to patients. PROMs measure this burden through patient questionnaires. They enable reporting of aspects that matter most to patients like subjective symptoms, quality of life, daily functioning and other aspects of their health and well-being. Finally, mounting evidence shows that lifestyle and psychosocial factors influence the course of the disease measured by classical clinical outcomes, but also the subjective perception of health, and therefore registration and reporting of these factors in every day practice is necessary.
By registering all outcomes and merging and analysing aggregated data in health care, new insights can arise that support the clinical decision-making process. Converting data into information can result in better management of patient and within the organization. To enable the transformation to data-driven health care, a cross-disciplinary model was developed at the MUMC+ (figure 2).
Who is involved?
Maastricht IBD-research group, Division 2, NUTRIM Maastricht University and Clinical IBD-team MUMC+: PI: Dr. M.J. Pierik, Prof dr. D. Jonkers , Dr. Z. Mujagic, Dr. J. Haans, Mrs. M. Cilissen, Mrs. I. Sour, Mr. M. Braun, Prof. dr. L. Stassen, Dr. S. Breukink, Dr. J Melenhorst, Dr. F. Kokke, Drs. N. Bevers, DataHub Maastricht University, Mr. P. Suppers, MyIBDcoach foundation, SMART-IBD network and Sananet bv.
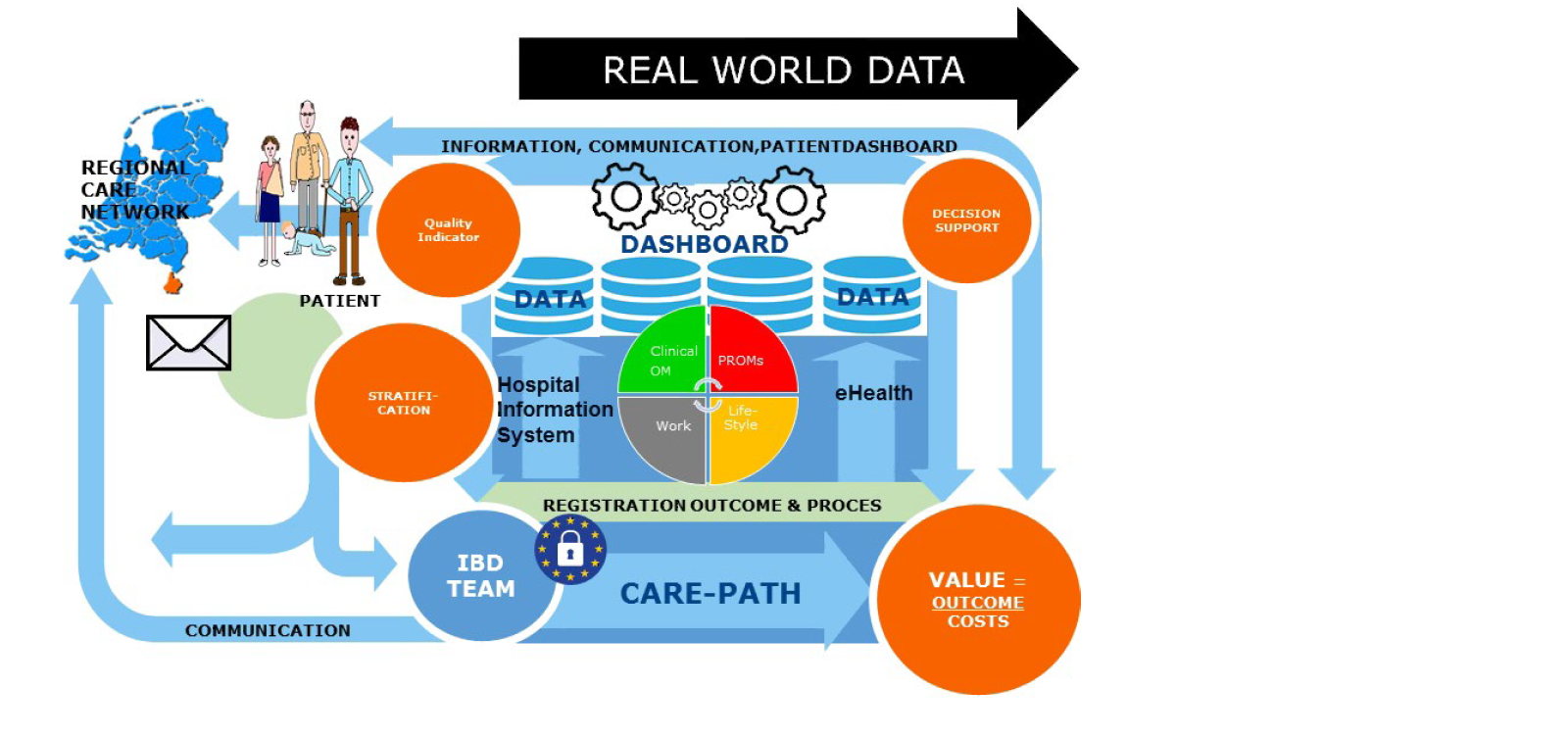
Referred patients from the regional care network are triaged to the optimal care path based on standardized data. During the first outpatient, patients are asked for permission to reuse data for multiple purposes. Standard sets of clinical outcome measures and process outcomes are registered during the primary care process in the Hospital Information system. PROMs, PREMs, psychosocial and lifestyle risk factors are registered in the eHealth tool myIBDcoach. Existing ZIBs are used as much as possible. Captured RWD is reused for:
- Shared decision-making in the consultation room with the aid of a patient dashboard and decision support tools.
- Patient group dashboards for evaluation and continuous improvement of the care path. Monitoring the balance between outcomes and costs.
- Communication within the regional care network.
- To provide quality indicators for external accountability and transparency.
- Development of decision support tools
- Optimization of patient stratification

Overview of the elements of the telemedicine tool myIBDcoach:
- Monitoring modules containing PROMS and clinical questionnaires: standard monitoring (every month, or every 3 months when the disease is in remission), intensified monitoring (weekly in case of a flare) and modules to prepare an outpatient clinc-visit.
- Personal Follow-up plan: Graphical visualisation of clinial outcomes, calprtectin point of care test, PROMs and psychosocial and lifestyle riskfactors in a dashboard for patients and health care professionals
- E-learning modules: interactive patient-tailored information on topics such as medications, adherence to medication, smoking cessation, (mal)nutrition, methods to prevent or reduce symptoms (self-management), fatigue, work productivity, anxiety and depression.
- Communication: secure message connection between patient and healthcare providers’ back-office.
Major breakthroughs
According to the literature and studies of the Maastricht IBD-research group in the IBD-South Limburg cohort, the most important cost drivers for IBD are diagnostics, outpatient clinic visits, hospitalisations, and medication. Based on this information, the classical IBD care-path was adapted into an eHealth care-path. A RCT shows that implementation of the eHealth care-path using myIBDcoach, resulted in a 50% reduction in hospitalisations and a 37% decrease of outpatient visits in one year. Patient reported treatment adherence and quality of life increased and quality of care was similar compared to standard care [4]. A cost–utility analysis shows that implementation of the registration of PROMs with telemedicine resulted in an average annual cost reduction of €547 per patient (95% CI, [€1029, €2143] and an increase in the cost-effectiveness ratio of €707 per patient (95% CI, [1241, 2544]) [5]. Further studies show that psychosocial factors (stress) and lifestyle factors (malnutrition) increase the risk of flares [6,7]. Moreover, an exploratory analysis shows that the predictive value of psychosocial and lifestyle factors for flares is higher than that of the classical clinical classification of IBD [8].
Scientific impact/Research quality
Selection recent publications
- Van den Heuvel TRA, Jeuring SFG, Zeegers MP, van Dongen DHE, Wolters A, Masclee AAM, Hameeteman WH, Romberg-Camps MJL, Oostenbrug LE, Pierik MJ, Jonkers DM. A 20-year temporal change analysis in incidence, presenting phenotype and mortality, in the Dutch IBDSL Cohort-can diagnostic factors explain the increase in IBD incidence? J Crohns Colitis. 2017;11(10):1169-79.
- Jeuring SF, van den Heuvel TR, Liu LY, Zeegers MP, Hameeteman WH, Romberg-Camps MJ, Oostenbrug LE, Masclee AA, Jonkers DM, Pierik MJ. Improvements in the long-term outcome of Crohn’s disease over the past two decades and the relation to changes in medical management: results from the population-based IBDSL cohort. Am J Gastroenterol. 2017;112(2):325-36.
- De Jong M, van der Meulen-de Jong A, Romberg-Camps M, Degens J, Becx M, Markus T, Tomlow H, Cilissen M, Ipenburg N, Verwey M, Colautti-Duijsens L, Hameeteman W, Masclee A, Jonkers D, Pierik M. Development and feasibility study of a telemedicine tool for all patients with IBD: MyIBDcoach. Inflamm Bowel Dis. 2017;23(4):485-93.
- De Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, Becx MC, Maljaars JP, Cilissen M, van Bodegraven AA, Mahmmod N, Markus T, Hameeteman WM, Dijkstra G, Masclee AA, Boonen A, Winkens B, van Tubergen A, Jonkers DM, Pierik MJ. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet. 2017;390(10098):959-68.
- de Jong MJ, Boonen A, van der Meulen-de Jong AE, Romberg-Camps MJ, van Bodegraven AA, Mahmmod N, Markus T, Dijkstra G, Winkens B, van Tubergen A, Masclee A, Jonkers DM, Pierik MJ. Cost-effectiveness of telemedicine-directed specialized vs standard care for patients with inflammatory bowel diseases in a randomized trial. Clin Gastroenterol Hepatol. 2020;18(8):1744-52.
- Spooren CEGM, Wintjens DSJ, de Jong MJ, van der Meulen- de Jong AE, Romberg-Camps MJ, Becx MC, Maljaars JP, van Bodegraven AA, Mahmmod N, Markus T, Hameeteman WM, Masclee AAM, Winkens B, Jonkers DMAE, Pierik MJ. Risk of impaired nutritional status and flare occurrence in IBD outpatients. Dig Liver Dis. 2019;51(9):1265-9.
- Wintjens DSJ, de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, Becx MC, Maljaars JP, van Bodegraven AA, Mahmmod N, Markus T, Haans J, Masclee AAM, Winkens B, Jonkers DMAE, Pierik MJ. Novel perceived stress and life events precede flares of inflammatory bowel disease: a prospective 12-month follow-up study. J Crohns Colitis. 2019;13(4):410-6.
- Lalisang RCA, Adriaans G, de Jong M, Van der Meulen-de Jong A, Romberg-Camps M, Mahmmod N, Markus-de Kwaadsteniet T, Dijkstra G, Haans J, Stamm C, Vanwersch R, Jonkers D, Almeida RJ, Pierik MJ, MyIBDcoach Study Group. Can lifestyle and psychosocial factors predict flares of IBD; an exploratory study using telemedicine. J Crohn’s Colitis. 2020;14:S059-60.
Users and collaborations
- The eHealth carepath with myIBDcoach is implmented in routine-care in 20 hospitals in the Netherlands.
- SMART-IBD is a learning network of health-care professionals (gastroenterologists, nurses, dieticians) of all 20 hospitals involved and the patient organisation (www.crohn-colitis.nl) with the aim to optimize care paths through smart registration and reusing outcomes via a Dataplatform (DataHub UM). Developing and evaluating care-paths that focus on interventions on psychosocial and lifestyle risk factors for chronic conditions are given special attention. The aim of the SMART-IBD collaboration is transition from monitoring classical outcomes and treatment of mucosal inflammation alone to improving health from the patient’s perspective.
Societal impact
With the myIBDcoach RCT - published in The Lancet in 2017 - the research group won the Wetenschaps- en Innovatieprijs of the Dutch federation for medical specialists (FMS).
The SMART-IBD project was nominated for the Value-Based Health Care Prize and the Zinnige Zorg Award.
By demonstrating that the eHealth care-path for IBD with, continuous monitoring of PROMs and psychosocial and lifestyle factors, is cost-effective compared to standard care, myIBDcoach could be implemented in 20 hospitals in the Netherlands. The data-optimized care paths for IBD are described in detail and shared with the SMART-IBD network. The SMART-IBD school aims to share knowledge regarding the innovative care-paths and organizes 3 monthly webinars for healthcare professionals.
Future perspectives
The SMART-IBD network is an ongoing collaboration using the aggregated data in DataHub UM to create evidence on life style and psychosocial interventions to prevent flares or improve health in IBD. The Maastricht IBD-research group maps myIBDcoach data to the OMOP common data model to enable combined analyses with the ICC-drug registry, PSI-IBD and IBD-SL cohort data to develop decision support tools and improve patient stratification of IBD.

