'It’s about behavioural change, which is a very complicated process'

The NIEZT project: towards improving infection prevention outside of the hospital
How can we improve infection prevention among health professionals in settings outside the hospital? That is the main question of research project NIEZT, a needs assessment for infection prevention among health professionals outside the hospital. To answer this question, CAPHRI researchers are working closely with healthcare practice. The project is being funded by LINK, the regional network for infection prevention and antibiotic resistance in Limburg.
“In hospital settings, the importance of infection prevention is very clear. If bacteria enter a wound, for example, it can easily get infected”, says Christian Hoebe, professor of Infectious Disease Control at CAPHRI and head of infectious disease control at Public Health Service South Limburg. It’s also clear why antibiotic resistance, which results in antibiotics losing their effectiveness, is dangerous for patients. This is why guidelines for infection prevention and the safe use of antibiotics tend to be properly observed in hospital settings. “It’s often different outside of the hospital. This project aims to identify the factors that impede the implementation of infection prevention and the factors that facilitate it. Even if guidelines for infection prevention are already in place, they are not always observed. Essentially”, says Christian Hoebe, “it’s primarily about behavioural change. And getting people to change their behaviour is a very complicated process. We want to find out what it takes.”
Involved research line
Involved Living Lab
Five healthcare sectors
Christian Hoebe is supervising PhD student Mitch van Hensbergen, a junior researcher at Public Health Service South Limburg who is doing his PhD research within the NIEZT project. The study began in 2018 in five different healthcare sectors in Limburg and Brabant: primary care (general practices), care and nursing homes, mental health care, and care for people with intellectual disabilities. The veterinary sector – veterinary surgeons and farmers – is also included in the study, and various municipal health services in Brabant and Limburg are involved. By now, Mitch van Hensbergen and his colleagues have interviewed dozens of professionals in these sectors. “From managers to nurses and from GPs to other health practitioners”, says the PhD student. As the study is still very much in progress, it’s too early to draw any conclusions. “But it is clear that sector-specific guidelines are needed, although there is a certain amount of overlap. In general, the severity of illness determines which guidelines are needed. Customisation is necessary, sometimes down to the location level, like in care settings for people with intellectual disabilities. For example, there certainly are ways to make people with mild intellectual disabilities aware of this problem and involve them in the solution.”
Partners
- GGD Zuid-Limburg
- GGD Limburg-Noord
- GGD Hart voor Brabant
- GGD West-Brabant
- National Institute for Public Health and the Environment (RIVM)/ LCI
- Vilans
High-priority concern
Moreover, there are differences between the various healthcare sectors, adds Christian Hoebe. Infection prevention is already a high-priority concern in care and nursing home settings, for example. And professionals providing care for people with intellectual disabilities are very willing to do more to prevent infections; various organisations in this sector are already working hard to step up their efforts. The mental healthcare sector is lagging behind in this respect. “Good hygiene practices, like washing your hands regularly, are necessary to prevent infections from spreading. But in mental health care, health professionals may not want the setting to be too ‘medical’”, says Casper den Heijer, doctor of Infectious Disease Control at Public Health Service South Limburg and Mitch van Hensbergen’s co-supervisor. Van Hensbergen adds, “There are also very practical concerns. In mental healthcare settings, for example, it’s not always possible to place hand sanitiser dispensers. Some clients with alcohol problems would drink from them, we were told.”
Questionnaires
As for general practice, GPs say that the infection prevention guidelines established by the Dutch College of General Practitioners tend to be properly observed, although there may be individual differences. GPs generally consider the risk of infectious disease transmission in general practices to be lower than in health facilities. The conclusion about the veterinary sector is that this is a very different world where professionals speak a very different language. “It was an interesting excursion for us and we definitely learnt from it”, says Christian Hoebe. “But our knowledge of this sector is too limited to be able to play a role in this. Our focus is on the other four (human) sectors.”
The results of the interviews are currently being translated into questionnaires. The researchers want to distribute these questionnaires in healthcare settings nationwide, starting with mental health care and care for people with intellectual disabilities. This will help them determine whether the impeding and facilitating factors cited by the interviewees are experienced all over the country. Based on the results, the sectors will be able to develop more specific guidelines. “It’s very practice-led research based on a theoretical question”, says Christian Hoebe. “This kind of approach increases the level of public support for the implementation of innovations. I also think that the COVID-19 pandemic is acting as a catalyst: it’s increasing awareness, which will make organisations more willing to invest in infection prevention. The social relevance is obvious: fewer infectious diseases.”
Text: Karin Burhenne
Translation: Emdash
More information:
NIEZT project
Project i-4-1-Health
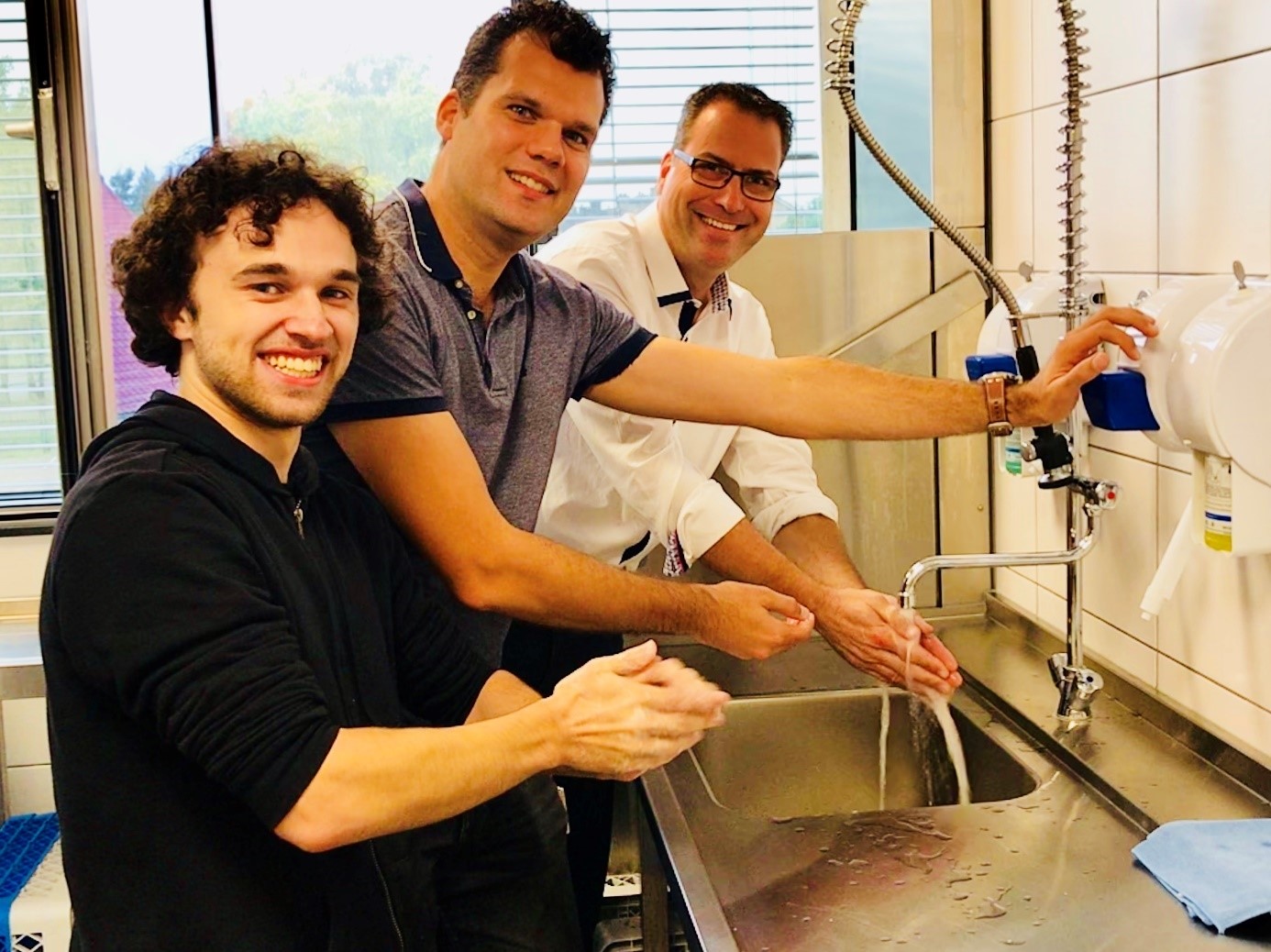
NIEZT project team: PhD candidate Mitch van Hensbergen, Dr. Casper den Heijer and Prof.dr. Christian Hoebe (picture taken before coronavirus outbreak)
